September 5 2025. doi: 0.5281/zenodo.17068744
Controlled breathing and its influence on anxiety and addiction in the heart and brain
Kevin P. Connelly, M.P.A.
Abstract
This study examined the physiological and psychological impact of guided breathwork on 65 participants. We measured changes in neural activity, autonomic balance, and subjective well-being. Results demonstrated an average 18.5% decrease in beta brain waves (associated with heightened thinking and anxiety) and a 23.8% increase in alpha waves (linked to relaxation and emotional regulation). Participants reached a state of heart coherence (defined as the synchronization of heart rate variability patterns with a balanced autonomic nervous system) within an average of 28.1 seconds. Physiologically, the average heart rate decreased by 7 beats per minute, with the largest individual drop recorded at 59 bpm. Self-reported outcomes showed that 93.4% experienced reduced anxiety and increased calm, while 98.5% expressed interest in continuing the practices. These findings suggest that short, structured breathwork interventions can rapidly induce coherence, reduce stress markers, and foster receptivity to ongoing practice.
Introduction
Over the past century, the way humans breathe has shifted dramatically. Research suggests that the average respiratory rate has increased from the slower, diaphragmatic breathing of earlier generations to a rapid 12–20 breaths per minute in the modern adult [1]. This trend toward chronic overbreathing does more than simply alter oxygen and carbon dioxide balance. It creates a physiological environment where the nervous system is held in a mild but persistent state of arousal, priming the body for anxiety and compulsive behavior [2].
Addiction and anxiety, though often treated as separate disorders, can be understood as two sides of the same coin. Both emerge when the nervous system is dysregulated and unable to return to balance. In this state, unconscious behavioral patterns take hold. Anxiety manifests as racing thoughts, hypervigilance, and agitation, while addiction channels the same dysregulation into repetitive actions that temporarily soothe the system [3].
The heart provides a reliable indicator of these internal states. When the nervous system is balanced, heart rhythms naturally fall into smooth, sine-wave patterns known as heart coherence [4]. This state reflects optimal communication between the heart and brain, allowing for emotional regulation and flexibility. The more time the body spends in coherence, the more capable it becomes of calming anxiety and resisting addictive urges. Conversely, when coherence is absent, the heart sends chaotic signals that reinforce stress, fear, and impulsivity [5].
Breathwork and heart rate variability (HRV)-based interventions have shown promise across multiple domains of addiction. In alcohol dependence, randomized trials have demonstrated that HRV biofeedback improves both short-term craving reduction [6] and long-term abstinence rates [7]. Similarly, pilot studies with young adults in inpatient settings found that brief HRV biofeedback sessions reduced craving and supported recovery [8]. Reviews support HRV biofeedback as a clinically relevant tool for substance use disorders [9].
Other addictions have also shown responsiveness to breath-based interventions. Breathing practices such as rhythmic pranayama have been associated with improvements in immune function and reductions in tobacco addiction [10]. Cigarette smoking itself has been linked with reduced HRV, underscoring the potential for breath-based approaches to restore autonomic regulation [11]. Breath interventions have been studied in relation to amphetamine use, where combining breathing-based practices with cognitive behavioral therapy enhanced treatment outcomes [12]. Resonance breathing has also been tested in women with substance use disorder, reducing both craving and negative affect [13].
Emerging work suggests that breath-based interventions may extend to food-related compulsions as well. Studies examining stress, craving, and autonomic regulation show that biofeedback and resonance breathing can alter the physiological states that underlie disordered eating and compulsive food use [14]. More broadly, chronic stress has been identified as a driver of both addictive vulnerability and relapse, with breathing practices offering a direct means to modulate this stress response [15].
Taken together, these findings highlight the central role of breath regulation in addiction recovery and anxiety. By restoring balance in both brain wave activity and heart rhythms, breathwork has the potential to reduce stress, increase emotional regulation, and improve impulse control. The current study expands on this foundation by measuring how guided breathwork affects brain activity, heart coherence, and self-reported wellbeing in adults across a wide age range.
Figure 1.
.png)
Methodology
Participants were guided through a structured 14-minute breathwork protocol while wearing EEG headsets from Muse to record brain wave activity and HRV monitors from the Heart Math Institute to track heart coherence. The session was divided into four phases: eyes open, eyes closed, guided breathing, and eyes closed integration. We then observed how different states of awareness and breathing patterns affected physiology. Data was collected in real time and later analyzed to compare changes across phases, highlighting shifts in neural activity and heart coherence directly linked to the breath practices. We used 7 different breathing exercises from the Reconnect Breath framework.
Figure 2.
.png)
Results
A total of 65 individuals participated in the intervention, with full datasets available for 47 participants. The sample included 29 women and 18 men, ranging in age from 25 to 69 years. Participants completed a guided breathwork session while data were collected using a Muse brain wave scanner and a HeartMath Institute emWave Pro heart rate variability monitor.
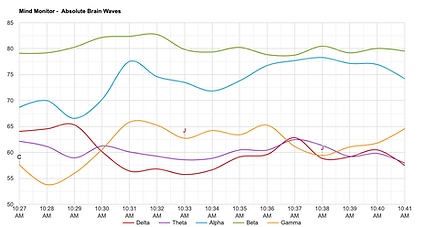
Analysis of brain wave activity indicated a significant shift in neural patterns following the intervention. The Muse device is a headband equipped with electroencephalography (EEG) sensors designed to measure electrical activity in the brain. For this study, Muse was used to track changes in beta and alpha wave activity. Beta waves are associated with mental activity, alertness, and stress, while alpha waves are linked with calmness, relaxed awareness, and emotional balance. The device outputs real-time frequency data, which were analyzed for percentage change across participants. Results showed an average 18.5 percent reduction in beta wave activity (SD = 4.6, range = 7–29 percent) and an average 23.8 percent increase in alpha activity (SD = 5.2, range = 12–34 percent). These data indicate that nearly all participants exhibited measurable shifts in brain activity during the session.
The shift observed here parallels the neurophysiological requirements for both reducing anxiety and weakening the compulsive drives characteristic of addiction. By decreasing beta-driven amygdala activation and supporting alpha-related regulation, the intervention appears to have directly influenced the neural mechanisms underpinning these two interrelated conditions.
Figure 3.
.png)
.png)
.png)
.png)
Cardiac measures reflected similar improvements. The emWave Pro, developed by the HeartMath Institute, measures heart rate variability (HRV) by detecting changes in the intervals between heartbeats through a pulse sensor placed on the ear. HRV patterns are analyzed by the software to determine levels of heart coherence, defined here as a smooth, sine-like wave pattern in heart rhythms representing balance between sympathetic and parasympathetic branches of the autonomic nervous system.
In this study, participants reached coherence within an average of 28.1 seconds (SD = 11.4). Heart rate also decreased across the sample, with an average reduction of 7 beats per minute (SD = 3.7). The smallest recorded change was 2 bpm, and the largest was a decrease of 59 bpm.Resting heart rate declined by an average of 7 beats per minute (SD = 3.7; range = 2–59). The largest individual decrease of 59 bpm was observed in a participant who entered with a highly elevated baseline rate, suggesting that the intervention can exert profound regulatory effects even under conditions of heightened arousal.
Figure 4.




Subjective data further supported the physiological findings. Post-session surveys indicated that 93.4% of participants reported reduced anxiety and increased calm, while 98.5% expressed interest in practicing these techniques again. Taken together, these results demonstrate that the intervention rapidly improved autonomic balance, shifted brain activity toward relaxed states, and produced strong self-reported benefits in mood and motivation to continue practice.
Discussion
The findings of this study demonstrate that even a single session of guided breathwork of just five minutes can rapidly shift both heart and brain activity into states associated with calm, emotional regulation, and self-control. The reduction in beta activity and the increase in alpha activity indicate a move away from cognitive hyperarousal and toward relaxed alertness. These neural patterns align with subjective reports of decreased anxiety and greater calm, suggesting that participants not only experienced measurable physiological changes but also recognized those changes internally [1,2].
One of the most notable outcomes was the speed with which participants entered heart coherence. On average, coherence was achieved in less than 30 seconds. Heart coherence reflects a harmonized pattern of heart rate variability, characterized by smooth, sine-like oscillations that indicate balance between sympathetic and parasympathetic branches of the autonomic nervous system [4]. This state is strongly associated with emotional stability, resilience, and the ability to regulate stress responses [5,6]. By entering coherence so quickly, participants demonstrated that slow, structured breathing can rapidly create the physiological foundation needed to calm anxiety and maintain control in the face of internal or external stressors.
The amygdala, the brain’s fear center, plays a central role in both anxiety and addiction. Faster, shallow breathing stimulates the amygdala, amplifying fear responses, increasing anxiety, and reducing impulse control [7]. It is also within the amygdala that many addictive patterns are reinforced [3]. By contrast, slow breathing decreases amygdala activity, reducing fear signaling and freeing the prefrontal cortex to exert greater executive control. The observed decrease in beta waves and increase in alpha waves is consistent with this neural shift, supporting the idea that breath regulation directly influences the brain’s capacity to manage cravings and resist compulsive behaviors [8,9].
From a behavioral standpoint, the overlap between anxiety and addiction is striking. Both can be seen as expressions of the same dysregulated nervous system state, where unconscious patterns take precedence over conscious choice. When participants reported reduced anxiety and increased calm after the session, it is likely that the same mechanisms reducing anxious arousal also enhanced their ability to manage urges. Previous studies using HRV biofeedback and breathwork interventions have demonstrated similar outcomes in populations with alcohol dependence [10,11], tobacco addiction [12,15], amphetamine use [14], and food-related compulsions [16]. In this way, slow breathing does not simply provide a temporary sense of relaxation, but rather restores the physiological conditions necessary for impulse control and long-term behavioral change.
The strong subjective endorsement of the practice, in which nearly all participants expressed a desire to continue, further underscores its potential utility. Sustained practice may not only reinforce these acute benefits but also gradually retrain the nervous system toward balance. Over time, repeated experiences of coherence and alpha-dominant brain activity may strengthen an individual’s baseline resilience, making them less vulnerable to both anxious states and addictive impulses [5,17].
These results add to a growing body of evidence that breathwork represents a powerful, accessible intervention for modern mental health challenges. Whereas many treatments for anxiety and addiction focus on cognitive or pharmacological approaches, breath-based practices directly target the underlying physiological states that drive both conditions [6,9,18]. The ability to measure outcomes through HRV and EEG adds a scientific foundation to practices that have long been a part of ancient healing traditions.
Taken together, this study suggests that structured breathwork is uniquely positioned to address the intertwined challenges of anxiety and addiction. By shifting both the heart and the brain into coherence and balance, slow breathing restores the conditions necessary for calm focus, emotional regulation, and conscious choice. These findings point toward breathwork as not just a wellness practice, but as a clinically relevant tool for addressing some of the most pressing psychological issues of modern society.
Limitations
Although the findings of this study provide promising evidence for the impact of breathwork on brain activity, heart coherence, and anxiety reduction, several limitations must be acknowledged. First, the sample size was modest, with complete data available from 47 participants. While the consistency of outcomes across individuals strengthens confidence in the results, larger samples will be needed to confirm generalizability and examine subgroup differences by age, gender, or baseline stress levels.
Second, the absence of a control group limits the ability to determine whether the observed effects can be attributed exclusively to the breathwork intervention. It is possible that nonspecific factors such as expectancy, novelty, or relaxation in a structured environment contributed to some of the reported benefits. Future research should incorporate randomized controlled designs comparing breathwork to other interventions or placebo conditions.
Third, the measures used (Muse EEG and HeartMath emWave Pro) provide accessible and practical means of assessing physiological change, but they are not equivalent to laboratory-grade equipment. While both tools have demonstrated validity for research and clinical applications, future studies may benefit from triangulating data with higher-resolution EEG and HRV systems to enhance precision and reliability.
Fourth, the study examined only immediate effects from a single five-minute session. Although results demonstrated rapid changes in both physiology and subjective state, it remains unclear how long these effects persist or whether they accumulate with regular practice. Longitudinal studies assessing daily or weekly practice over months would help clarify whether repeated breathwork can lead to enduring improvements in emotional regulation and reductions in addictive tendencies.
Finally, the study did not examine potential differences in effectiveness based on type of addiction, severity of anxiety, or other psychosocial variables. Given the evidence supporting breath and HRV-based interventions in alcohol [10,11], tobacco [12,15], amphetamine [13], and food-related compulsions [16], future research should tailor protocols to specific populations and compare outcomes across conditions.
In sum, while this study highlights the potential of breathwork to rapidly influence both physiological and psychological markers of wellbeing, further research is needed to confirm these findings in larger, more diverse samples and to determine the long-term clinical significance of these effects.
References
1. Courtney, R. (2009). The functions of breathing and its dysfunctions and their relationship to breathing therapy. International Journal of Osteopathic Medicine, 12(3), 78–85. https://doi.org/10.1016/j.ijosm.2009.04.002
2. Gilbert, C. (2003). Clinical applications of breathing regulation. Behavior Modification, 27(5), 692–709. https://doi.org/10.1177/0145445503256321
3. Sinha, R. (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141(1), 105–130. https://doi.org/10.1196/annals.1441.030
4. McCraty, R., Atkinson, M., & Tomasino, D. (2009). Coherence: Bridging personal, social, and global health. Alternative Therapies in Health and Medicine, 15(4), 10–24.
5. McCraty, R., & Zayas, M. A. (2014). Cardiac coherence, self-regulation, autonomic stability, and psychosocial well-being. Frontiers in Psychology, 5, 1090. https://doi.org/10.3389/fpsyg.2014.01090
6. Lehrer, P. M. (2019). Heart rate variability biofeedback and other psychophysiological procedures as important elements in psychotherapy. International Journal of Psychophysiology, 131, 89–95. https://doi.org/10.1016/j.ijpsycho.2018.08.008
7. Sloan, S. A., Hallgren, K. A., & Witkiewitz, K. (2021). Effects of arousal modulation via resonance breathing on craving and affect among women with substance use disorder: A preliminary randomized crossover trial. Addictive Behaviors, 123, 107059. https://doi.org/10.1016/j.addbeh.2021.107059
8. Eddie, D., Kim, C., Lehrer, P., Deneke, E., & Bates, M. E. (2014). A pilot study of brief heart rate variability biofeedback to reduce craving in young adult men receiving inpatient treatment for substance use disorders. Applied Psychophysiology and Biofeedback, 39(3-4), 181–192. https://doi.org/10.1007/s10484-014-9251-z
9. Leyro, T. M., Buckman, J. F., & Bates, M. E. (2019). Theoretical implications and clinical support for heart rate variability biofeedback for substance use disorders. Current Opinion in Psychology, 30, 92–97.
https://doi.org/10.1016/j.copsyc.2019.03.008
10. Penzlin, A. I., Siepmann, T., Illigens, B. M., Weidner, K., & Siepmann, M. (2015). Heart rate variability biofeedback in patients with alcohol dependence: A randomized controlled study. Neuropsychiatric Disease and Treatment, 11, 2619–2627. https://doi.org/10.2147/NDT.S84798
11. Penzlin, A. I., Barlinn, K., Illigens, B. M. W., et al. (2017). Effect of short-term heart rate variability biofeedback on long-term abstinence in alcohol dependent patients – a one-year follow-up. BMC Psychiatry, 17, 325. https://doi.org/10.1186/s12888-017-1480-2
12. Kochupillai, V., Kumar, P., Singh, D., Aggarwal, D., Bhardwaj, N., Bhutani, M., & Das, S. N. (2005). Effect of rhythmic breathing (Sudarshan Kriya and Pranayam) on immune functions and tobacco addiction. Annals of the New York Academy of Sciences, 1056(1), 242–252. https://doi.org/10.1196/annals.1352.039
13. Recovery Research Institute. (2020, April 15). A breathing-based intervention may enhance benefits of cognitive behavioral therapy for individuals with amphetamine use disorder. Retrieved from https://www.recoveryanswers.org/research-post/breathing-based-intervention-enhance-benefits-cognitive-behavioral-therapy-amphetamine-disorder/
14. Eddie, D., Price, J. L., Bates, M. E., & Buckman, J. (2021). Substance use and addiction affect more than the brain: The promise of neurocardiac interventions. Current Addiction Reports, 8(3), 431–439. https://doi.org/10.1007/s40429-021-00379-3
15. Bodin, F., McIntyre, K. M., Schwartz, J. E., McKinley, P. S., Cardetti, C., Shapiro, P. A., Gorenstein, E., & Sloan, R. P. (2017). The association of cigarette smoking with high-frequency heart rate variability: An ecological momentary assessment study. Psychosomatic Medicine, 79(9), 1045–1050. https://doi.org/10.1097/PSY.0000000000000507
16. Liu, S., Oshri, A., & Duprey, E. B. (2020). Heart rate variability reactivity moderates the indirect link between child maltreatment and young adult alcohol use problems via depressive symptoms. The American Journal on Addictions, 29(2), 141–150. https://doi.org/10.1111/ajad.13004
17. Jørgensen, M. A., Pallesen, K. J., Fjorback, L. O., & Juul, L. (2021). Effect of mindfulness-based stress reduction on dehydroepiandrosterone-sulfate in adults with self-reported stress: A randomized trial. Clinical and Translational Science, 14(6), 2360–2369. https://doi.org/10.1111/cts.13100
18. Eddie, D., Price, J. L., Bates, M. E., & Buckman, J. (2021). Substance use and addiction affect more than the brain: The promise of neurocardiac interventions. Current Addiction Reports, 8(3), 431–439. https://doi.org/10.1007/s40429-021-00379-3